Acute Kidney Injury
Common in hospitalized patients, increasing in incidence, and associated with adverse outcomes. But, hard to identify.
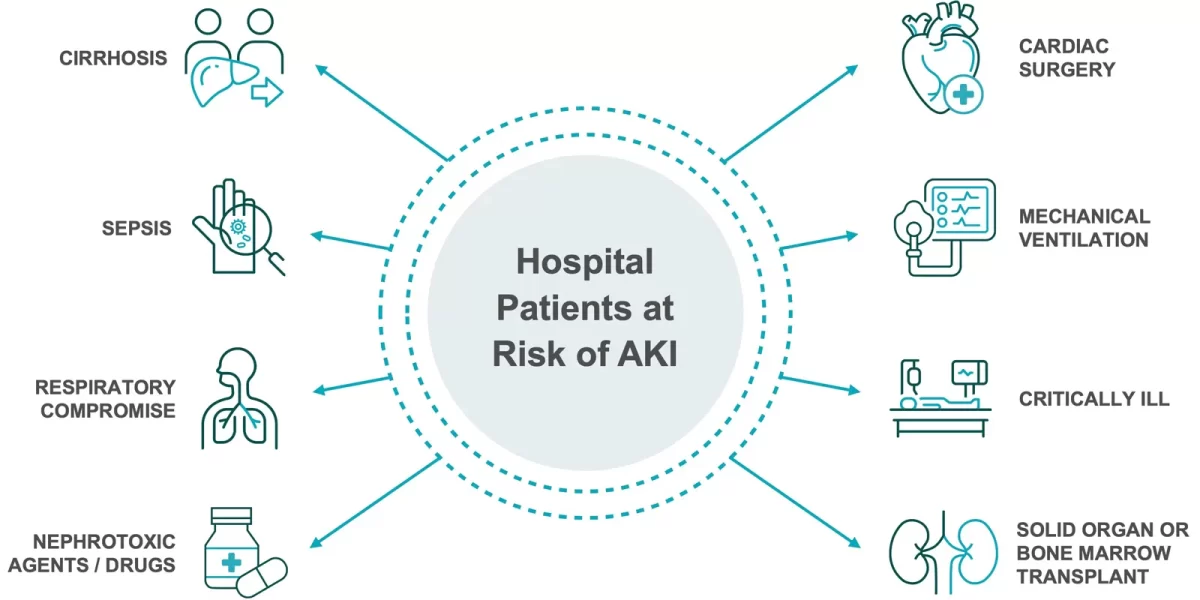
AKI Risk Factors
Acute kidney injury (AKI) is a rapid loss of kidney function, which typically happens as a complication of another serious illness or intervention. Because pain and other symptoms don’t usually occur, rapid identification of patients who are at riski is critical, as there is no specific treatment for AKI.
Identify AKI earlier with The NGAL Test.
AKI is Associated with Adverse, Long-Term Outcomes
1 in 5
Hospitalized patients at riskii
+7 to 23
Days in hospitaliii
Overall mortality rateiv
AKI survivors with one or more kidney abnormalitiesv
AKI Classification Systems
The definition of AKI, previously known as acute renal failure (ARF), has evolved for nearly two decades, as clinicians have struggled to classify the condition.vi
Developed in 2012, the current KDIGO definition and staging of AKIvii are summarized here. These guidelines are under review with updates expected in 2026.
KDIGO - Kidney Disease Improving Global Outcomes Criteria
| Stage | Serum Creatinine | Urine Output |
|---|---|---|
| 1 | 1.5–1.9 times baseline,or ≥0.3 mg/dL >26.5 µmol/L increase | <0.5 mL/kg/h for 6-12h |
| 2 | 2–2.9 times baseline | <0.5 mL/kg/h for ≥12h |
| 3 | 3 times baseline, OR Increase in serum creatinine to ≥4 mg/dL, OR Initiation of renal replacement therapy | <0.3 mL/kg/h for ≥24h, or anuria for ≥12h |
Receive AKI Guideline Updates
Stay up to date on the latest kidney care guideline updates. We’ll issue them as they become available.
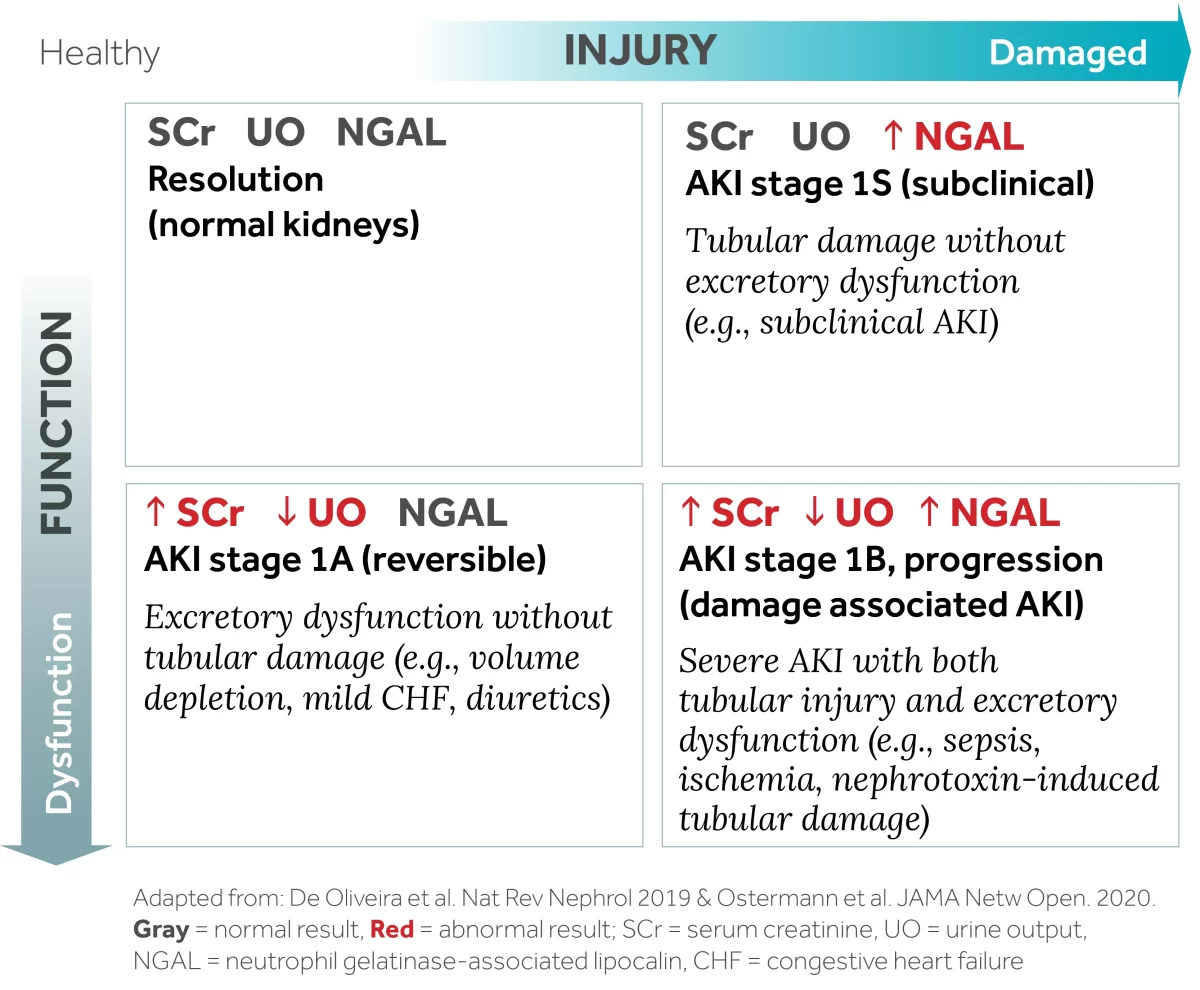
AKI Assessment Using Functional and Damage Biomarkers
In 2020, the Acute Disease Quality Initiative (ADQI) workgroup recommended that “a combination of damage and functional biomarkers, along with clinical information, be used to improve the diagnostic accuracy of AKI, to recognize the different pathophysiological processes, to discriminate AKI etiology, and to assess AKI severity.”viii
Neutrophil gelatinase-associated lipocalin (NGAL) is a renal damage biomarker with extensive research in different patient populations and clinical settings.
What is Acute Kidney Injury (AKI)?
AKI is an abrupt loss of kidney function that develops rapidly over a few hours or days, defined by KDIGO as an increase in creatinine by more than 0.3 mg/dl within 48 hours or a reduction in urine volume to less than 0.5ml/kg/hour for 6 hours.i Learn more about AKI.
How common is AKI?
AKI is a silent epidemic that affects 13.3 million patients worldwide.ii It affects 10-15% of hospitalized patients, and 25-57% of those in intensive care units.iii Episodes of in-hospital AKI are steadily increasing – the U.S. saw an increase of 29% in the period from 2011-2021.iv
What are the risk factors for AKI?
AKI is a diverse clinical spectrum. Patients with the highest risk of developing AKI in a hospital setting include those undergoing cardiac surgery (up to 30%)v, on mechanical ventilation for respiratory support (29%)vi and those receiving nephrotoxic medications (14-26%)vii. Other AKI risk factors include sepsis, multiple organ failure and solid organ or bone marrow transplant.viii Patients with diabetes and chronic kidney disease are also at greater risk of developing AKI.ix
How serious is AKI?
AKI is associated with prolonged length of stay in the ICU and hospital, as well as poorer outcomes. Increased AKI severity and duration correlates with increased morbidity, the need for dialysis, prolonged time on mechanical ventilation and increased mortality.x Annually, AKI contributes to as many as 1.7 million deaths globally.xi
What are the long term consequences of AKI?
One to five years post-discharge, individuals who have had even one episode of AKI have been found to have a 30% higher rate of hospital re-admissionxii, are 38% more likely to have a major cardiac eventxiii and 25% progress to chronic kidney diseasexiv.
Why is AKI difficult to identify early?
AKI is frequently asymptomatic and painless, and is often a complication of another illness or surgery. The standard definition of AKI is based on a change in serum creatinine (SCr) levels and urine output (UO). SCr and UO are measures of kidney function, not kidney damage. Functional changes reflective of AKI are not detectable until 48 to 72 hours after kidney damage begins.xv
Is AKI preventable?
AKI can be hard to predict or prevent. The earlier AKI or risk of AKI is identified, the sooner clinical action can be taken to mitigate or prevent permanent kidney damage. Understanding the risk factors for AKI is important, and the addition of damage biomarkers like NGAL provides another data point for clinicians to consider in their clinical assessment.xvi
AKI in lower-middle income countries is considered largely preventable with public health initiatives such as improved sanitation and water hygiene, education, and access to healthcare.xvii
How does AKI impact healthcare systems?
It is estimated that acute kidney injury costs a health system an additional $7,000 per episodexviii and $5-$20 billion annually.xix AKI can impact re-hospitalization rates and long-term patient health, necessitating additional healthcare utilization.
References
iKhwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179-c184.
iiMehta RL, Cerdá J, Burdmann EA, et al. International Society of Nephrology's 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet. 2015;385(9987):2616-2643.
iiiHoste EA, Bagshaw SM, Bellomo R, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41(8):1411-1423.
ivUnited States Renal Data System. 2023 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2023.
vO'Neal JB. Acute kidney injury following cardiac surgery: Current understanding and future directions. Crit Care. 2016;20(1).
viLombardi R. et al. An assessment of the Acute Kidney Injury Network creatinine-based criteria in patients submitted to mechanical ventilation. Clin J Am Soc Nephrol. 2011;6(7).
viiAlobaidi R. et al. Sepsis-associated acute kidney injury. Semin Nephrol. 2015;35(1).
viiiRonco C, Bellomo R, Kellum JA. Acute kidney injury. Lancet. 2019;394(10212):1949-1964.
ixHapca S, Siddiqui MK, Kwan RSY, et al. The Relationship between AKI and CKD in Patients with Type 2 Diabetes: An Observational Cohort Study. J Am Soc Nephrol. 2021;32(1):138-150.
xHoste EAJ, Kellum JA, Selby NM, et al. Global epidemiology and outcomes of acute kidney injury. Nat Rev Nephrol. 2018;14(10):607-625.
xiLewington AJ, Cerdá J, Mehta RL. Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney Int. 2013;84(3):457-467.
xiiHessey E. et al. Healthcare Utilization after Acute Kidney Injury in the Pediatric Intensive Care Unit. Clin J Am Soc Nephrol, 2018;13(5).
xiiiOdutayo A. et al. AKI and Long-Term Risk for Cardiovascular Events and Mortality. JASN. 2017;28(1).
xivHorne KL. et al. Three-year outcomes after acute kidney injury: results of a prospective parallel group cohort study. BMJ Open. 2017;7(3).
xvMoledina DG, Parikh CR. Phenotyping of Acute Kidney Injury: Beyond Serum Creatinine. Semin Nephrol. 2018;38(1):3-11.
xviOstermann M, Zarbock A, Goldstein S, et al. Recommendations on Acute Kidney Injury Biomarkers From the Acute Disease Quality Initiative Consensus Conference: A Consensus Statement JAMA Netw Open. 2020;3(10):e2019209.
xviiKellum JA, Romagnani P, Ashuntantang G, Ronco C, Zarbock A, Anders HJ. Acute kidney injury. Nat Rev Dis Primers. 2021;7(1):52.
xviiiSilver SA, Chertow GM. The Economic Consequences of Acute Kidney Injury. Nephron. 2017;137(4):297-301.
xixSilver SA, Long J, Zheng Y, Chertow GM. Cost of Acute Kidney Injury in Hospitalized Patients. J Hosp Med. 2017;12(2):70-76.
xxDevarajan P. Neutrophil gelatinase-associated lipocalin: a promising biomarker for human acute kidney injury. Biomark Med. 2010;4(2):265–280.
i Ronco C, Bellomo R, Kellum JA. Acute kidney injury. Lancet. 2019;394(10212):1949-1964.
iiSusantitaphong P, Cruz DN, Cerda J, et al. World incidence of AKI: a meta-analysis. Clin J Am Soc Nephrol. 2013;8(9):1482–1493.
iiiSutherland SM, Ji J, Sheikhi FH, Widen E, Tian L, Alexander SR, Ling XB. AKI in hospitalized children: epidemiology and clinical associations in a national cohort. Clin J Am Soc Nephrol. 2013 Oct;8(10):1661-9.
ivMehta RL, Cerdá J, Burdmann EA, et al. International Society of Nephrology's 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet. 2015;385(9987):2616-2643.
vAskenazi DJ, Feig DI, Graham NM, Hui-Stickle S, Goldstein SL. 3-5 year longitudinal follow-up of pediatric patients after acute renal failure. Kidney Int. 2006;69(1):184-189.
viKellum JA, Levin N, Bouman C, Lameire N. Developing a consensus classification system for acute renal failure. Curr Opin Crit Care. 2002;8(6):509-514.
viiKhwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179-c184.
viiiOstermann M, Zarbock A, Goldstein S, et al. Recommendations on Acute Kidney Injury Biomarkers From the Acute Disease Quality Initiative Consensus Conference: A Consensus Statement JAMA Netw Open. 2020;3(10):e2019209.
